Abstract
Background: Studying the impact of race/ethnicity on stem cell transplant outcomes helps us improve health care disparities and access to transplant. The use of umbilical cord blood (UCBT) was designed to allow mismatched UCB units and improve access to transplant for patients lacking a fully matched donor. Previous CIBMTR studies (Ballen et al, BBMT, 2012) showed that Black patients had a lower overall survival (OS) than White patients following single UCBT; however, outcomes were similar when UCB units of comparable cell dose and HLA match were used. The current study draws on a larger, more modern cohort and compares outcomes among non-Hispanic White (White), non-Hispanic Black (Black), Hispanic/Latinx (Latinx) and Asian patients.
Methods: CIBMTR data from 2007 to 2017 were used. Patients were between ages 1 and 80; 983 received single and 1259 double UCBT, following either a myeloablative (N=1752) or reduced intensity conditioning (N=759). The primary outcome was OS at 2 years, which was estimated using the Kaplan-Meier method with the log-rank test used for univariate comparisons. Secondary outcomes included disease free survival, transplant related mortality (TRM), acute and chronic graft vs host disease (GVHD), and GVHD free, relapse free survival (GRFS). Multivariate analysis was performed to determine factors associated with outcomes and whether race/ethnicity influences these outcomes.
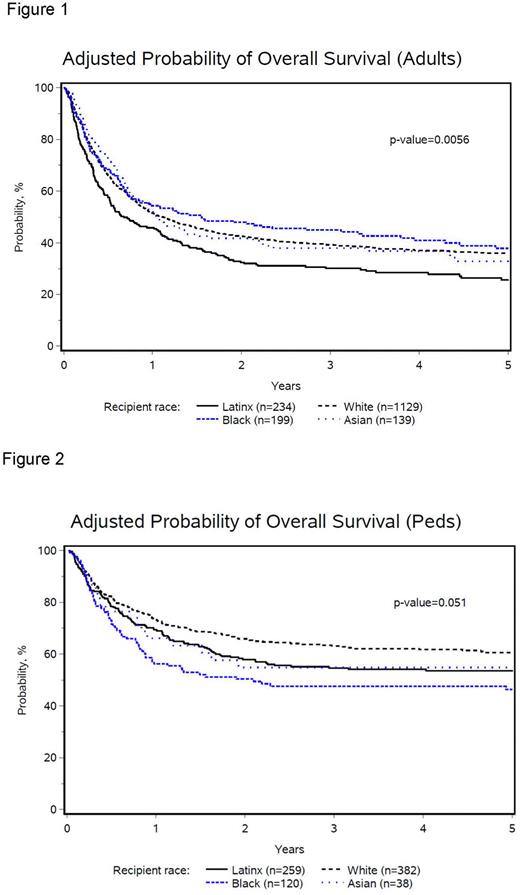
Results: A total of 1705 adults and 807 children were included. For adults, in univariate analysis, 2-year OS was 41.5% (99% CI, 37.6-45.3) for Whites, 36.1% (99% CI, 28.2-44.5) for Latinx, 45.8% (99% CI, 36.7-55.1) for Blacks, and 44.5% (99% CI, 33.6-55.6) for Asians. In multivariate analysis of adults, Latinx patients had inferior OS compared to other racial/ethnic groups (p=0.005) (Figure 1). OS improved over time across all racial/ethnic groups (p=0.009; 2016-2017 vs. 2007-2009 HR 0.68, 99% CI 0.51-0.91). Relapse and TRM rates were higher in Latinx compared to other groups but did not reach statistical significance. GVHD rates were comparable among the different racial/ethnic groups. There was no survival advantage to receiving a UCB unit from a donor of similar race/ethnicity, for any racial/ethnic groups
In children, the 2-year OS in univariate analysis was 66.1% (99% CI, 59.7-72.2) for Whites, 57.1% (99%CI, 49-64.9) for Latinx, 46.8% (99%CI, 35.3-58.4) for Blacks, and 53.8% (99%CI, 32.7-74.2) for Asians. In multivariate analysis of children, no difference in OS was observed among racial/ethnic groups (p = 0.05) (Figure 2). Similarly, there was no difference in relapse (p=0.40) and TRM rates (p=0.14). Grade 3-4 Acute GVHD was higher in Blacks compared with Whites (p= 0.0016, HR 2.25, 99% CI 1.36-3.74). There was no survival advantage to receiving a UCB unit from a donor of similar race/ethnicity, for any racial/ethnic groups.
Conclusion: 1. UCBT provides a donor for diverse patients. 2. In adults, OS has improved over time for all racial/ethnic groups. 3. In adults, OS is comparable among Whites, Blacks, and Asians and lower for Latinx patients. 4. In children, OS is comparable among Whites, Blacks, Latinx, and Asians. 5. In children, Grade 3 and 4 acute GVHD was higher in Black patients. 6.There was no survival benefit to matching UCB unit and patient by race/ethnicity for adults and children, although the numbers were small in the non-White cohorts.
As our study reveals race/ethnicity matching has minimal to no impact on outcomes post UCB transplant it may be advantageous for UCB banks to target collection of larger units over race/ethnicity quotas. Future studies will study biologic or socioeconomic explanations for the lower OS in adult Latinx patients and the higher acute GVHD in pediatric black patients.
Disclosures
Wood:Pfizer: Research Funding; Genentech: Research Funding; Teladoc: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal